Pain Management
Effective Wisdom Tooth Surgery Recovery Strategies
Essential Wisdom Tooth Removal Aftercare Tips
Understanding the Process
So, you’ve just had your wisdom teeth removed. It’s a common procedure, but the aftercare is crucial for a smooth recovery. Wisdom teeth, also known as third molars, often cause issues like pain, overcrowding, and infections when they emerge. Removing them can alleviate these problems and prevent future complications.
Immediate Post-Op Care
Right after the procedure, your mouth will likely be numb from the anesthesia. It’s essential to follow your dentist’s instructions carefully during this time. They may recommend biting down gently on gauze pads to control bleeding and reduce swelling. Applying an ice pack to the outside of your face can also help minimize swelling and discomfort.
Managing Pain and Discomfort
Pain and discomfort are common after wisdom tooth removal. Your dentist may prescribe pain medication or recommend over-the-counter options like ibuprofen. It’s essential to take these medications as directed to manage your pain effectively. Additionally, sticking to a soft diet and avoiding spicy or acidic foods can help prevent irritation and discomfort.
Controlling Bleeding
Some bleeding is normal after wisdom tooth removal, but excessive bleeding can be a cause for concern. To control bleeding, gently bite down on gauze pads placed over the extraction sites. Change the gauze pads as needed and avoid vigorous rinsing or spitting, as this can dislodge blood clots and prolong bleeding. If bleeding persists, contact your dentist immediately.
Preventing Infection
Reducing the risk of infection is crucial during the recovery period. Your dentist may prescribe antibiotics to prevent or treat any potential infections. Additionally, rinsing your mouth gently with warm salt water several times a day can help keep the extraction sites clean and reduce the risk of infection. Be sure to follow any specific instructions provided by your dentist regarding oral hygiene.
Managing Swelling
Swelling is a common side effect of wisdom tooth removal and can be uncomfortable. Applying an ice pack to the outside of your face for 20 minutes on, 20 minutes off, can help reduce swelling and discomfort. It’s essential to keep your head elevated while resting to further minimize swelling. If swelling persists or worsens, contact your dentist for further guidance.
Maintaining Proper Oral Hygiene
While it’s essential to keep the extraction sites clean, it’s also crucial to maintain proper oral hygiene throughout the recovery process. Brush your teeth gently, being careful to avoid the extraction sites, for the first few days after surgery. You can resume normal brushing and flossing once your dentist gives you the green light. However, be gentle around the extraction sites to avoid irritation or damage.
Eating a Soft Diet
In the days following wisdom tooth removal, sticking to a soft diet can help prevent discomfort and irritation. Opt for foods like soups, yogurt, mashed potatoes, and smoothies that are easy to chew and swallow. Avoid hard, crunchy, or spicy foods that could irritate the extraction sites or dislodge blood clots.
Attending Follow-Up Appointments
After wisdom tooth removal, your dentist will likely schedule a
Ensuring Comfort: Excellence in Anesthesia Care

Ensuring Comfort: Navigating the Realm of Anesthesia Care
In the realm of medical interventions, the provision of anesthesia care stands as a crucial element, ensuring patient comfort, safety, and pain management. This intricate field combines medical expertise, precise administration of medications, and vigilant monitoring to create a secure environment for individuals undergoing various medical procedures. Let’s delve into the multifaceted aspects of anesthesia care, exploring its significance and the commitment to patient well-being.
The Art and Science of Sedation: Anesthesia’s Fundamental Role
Anesthesia care is often described as the art and science of inducing a controlled state of unconsciousness or sedation to facilitate medical procedures. The fundamental goal is to ensure patients are free from pain, anxiety, and awareness during surgical or medical interventions. Anesthesia care is not a one-size-fits-all approach; instead, it is tailored to the specific needs of each patient and the nature of the procedure.
Preoperative Assessment: Tailoring Anesthesia Plans
The journey of anesthesia care begins with a comprehensive preoperative assessment. Anesthesiologists evaluate the patient’s medical history, current health status, and any pre-existing conditions to formulate an anesthesia plan. This tailored approach considers factors such as age, overall health, allergies, and the type of procedure to determine the most appropriate anesthesia technique.
Informed Consent and Patient Education: Building Trust
An essential component of anesthesia care is obtaining informed consent. Anesthesiologists engage in patient education, explaining the planned anesthesia approach, potential risks, and expected outcomes. Building trust through clear communication is paramount, empowering patients to make informed decisions about their anesthesia care. Informed consent is a collaborative process that enhances patient understanding and contributes to a positive anesthesia experience.
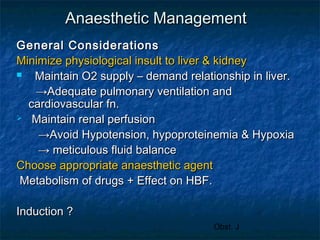
Anesthetic Administration: Precision and Safety
The administration of anesthesia involves a delicate balance of medications to induce and maintain the desired level of sedation. Anesthesiologists carefully select and administer anesthetic agents, continuously monitoring vital signs such as heart rate, blood pressure, and oxygen levels. This precision ensures the patient remains in a controlled and safe state throughout the procedure.
Types of Anesthesia: Tailoring to Patient Needs
Anesthesia care encompasses various types of anesthesia tailored to meet individual patient needs and the nature of the medical procedure. General anesthesia induces a reversible state of unconsciousness, while regional anesthesia targets specific regions of the body, providing pain relief for localized procedures. Local anesthesia is employed for minor procedures, numbing a specific area without affecting consciousness. The choice of anesthesia type is a collaborative decision based on medical considerations and patient preferences.
Intraoperative Monitoring: Safeguarding Patient Well-Being
Anesthesia care includes vigilant intraoperative monitoring to safeguard patient well-being. Anesthesiologists continuously assess vital signs, adjust anesthesia levels as needed, and respond promptly to any changes in the patient’s condition. This proactive monitoring ensures real-time adjustments to maintain optimal anesthesia depth and address any emerging challenges during the procedure.
Postoperative Care and Recovery: Transitioning to Consciousness
The role of anesthesia care extends into the postoperative period. Anesthesiologists oversee the transition of patients from the anesthetized state to consciousness. Postoperative care involves monitoring for the emergence
Navigating Anesthesia: Best Practices for Patient Care
Navigating Anesthesia: Best Practices for Patient Care
Anesthesia practices play a critical role in ensuring patient comfort and safety during medical procedures. In this article, we will explore the key components of anesthesia practices, highlighting the importance of adherence to best practices for optimal patient outcomes.
Precision in Preoperative Assessment
Anesthesia practices commence with a thorough preoperative assessment. This crucial step involves evaluating the patient’s medical history, current health status, and any potential risks or complications. A precise understanding of the patient’s condition allows anesthesia providers to tailor the anesthetic plan to individual needs, minimizing risks and ensuring a smooth intraoperative experience.
Tailoring Anesthetic Plans to Patient Needs
Best practices in anesthesia involve tailoring anesthetic plans to the specific needs of each patient. Factors such as age, medical history, and the type of surgical procedure guide the selection of anesthetic agents and techniques. This personalized approach ensures that patients receive the most appropriate and effective anesthesia for their unique circumstances.
Informed Consent and Patient Communication
Ensuring informed consent is a fundamental best practice in anesthesia. Anesthesia providers communicate with patients, explaining the anesthesia plan, potential risks, and expected outcomes. This open dialogue fosters trust and allows patients to make informed decisions about their care. Effective communication is key to addressing patient concerns and ensuring a positive perioperative experience.
Monitoring Vital Signs and Patient Safety
Throughout the anesthesia process, continuous monitoring of vital signs is paramount. Best practices involve vigilant oversight of parameters such as heart rate, blood pressure, oxygen saturation, and end-tidal carbon dioxide. These measures provide real-time information about the patient’s physiological status, enabling immediate intervention if any abnormalities arise.
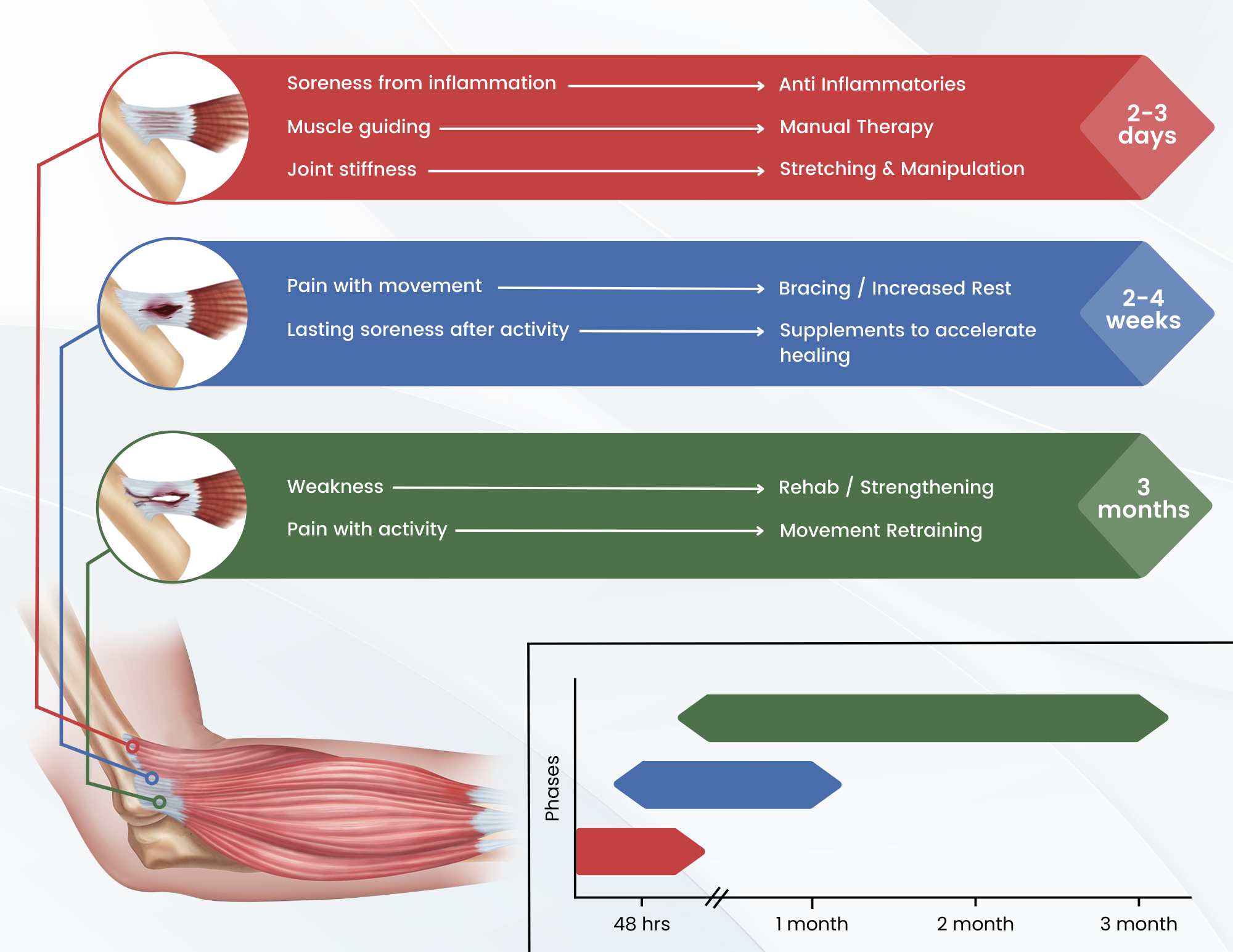
Pain Management Strategies
Anesthesia practices extend to postoperative pain management. Anesthesia providers collaborate with other healthcare professionals to develop comprehensive pain management strategies. This may involve a combination of pharmacological interventions, regional anesthesia techniques, and non-pharmacological approaches to ensure optimal pain relief while minimizing side effects.
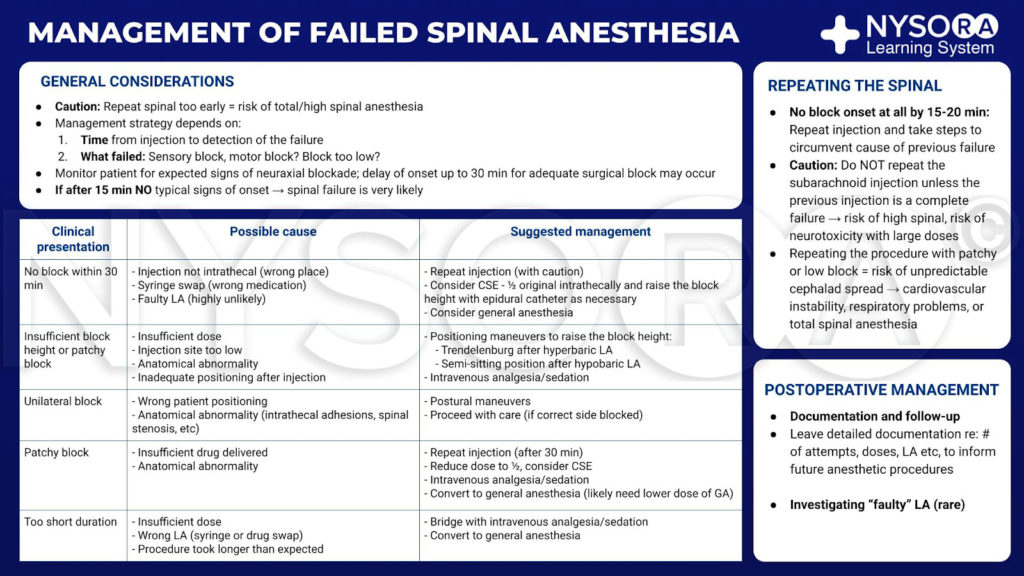
Emergency Preparedness and Crisis Management
Best practices in anesthesia include robust emergency preparedness and crisis management. Anesthesia providers undergo regular training to respond swiftly and effectively to unexpected complications. This preparedness extends to equipment checks, resuscitation protocols, and coordination with the surgical team to address emergencies seamlessly and safeguard patient well-being.
Adherence to Infection Control Protocols
Infection control is a critical aspect of anesthesia practices. Anesthesia providers adhere to strict protocols to prevent the transmission of infections. This involves maintaining a sterile environment, proper hand hygiene, and meticulous care in handling equipment and medications. These practices contribute to reducing the risk of surgical site infections and other complications.
Continuous Professional Development
Staying abreast of advancements in anesthesia is a best practice embraced by anesthesia providers. Continuous professional development involves attending conferences, engaging in ongoing education, and staying informed about new technologies and research findings. This commitment ensures that anesthesia practices align with the latest evidence-based approaches, enhancing patient care.
Collaboration with Multidisciplinary Teams
Best practices in anesthesia emphasize collaboration with multidisciplinary healthcare teams. Anesthesia providers work closely with surgeons, nurses, and other specialists
Precision in Sedation: Anesthesia Management Mastery
Precision in Sedation: Anesthesia Management Mastery
Effective anesthesia management is a cornerstone of patient safety and comfort during medical procedures. In this article, we delve into the intricate world of anesthesia management, exploring the key components, safety measures, and the expertise required to ensure precision in sedation.
Patient Assessment and Individualized Plans
Anesthesia management begins with a thorough patient assessment. Anesthesiologists evaluate medical history, current health status, and any potential risks. Individualized anesthesia plans are then crafted, taking into account factors such as age, existing medical conditions, and the specific procedure requirements. This personalized approach enhances safety and optimizes sedation outcomes.
Selection and Administration of Anesthetic Agents
The choice and administration of anesthetic agents are critical aspects of anesthesia management. Anesthesiologists select the most suitable drugs based on the patient’s needs and the nature of the procedure. Precision in dosage and monitoring ensures that patients receive the right level of sedation while minimizing the risk of adverse effects.
Continuous Monitoring and Adjustments
During procedures, continuous monitoring is paramount. Anesthesia management involves vigilant tracking of vital signs, including heart rate, blood pressure, and oxygen levels. Anesthesiologists make real-time adjustments to the anesthesia delivery to maintain the desired level of sedation and respond promptly to any changes in the patient’s condition.
Airway Management and Ventilation
Ensuring a patent airway and proper ventilation is a fundamental responsibility in anesthesia management. Anesthesiologists employ various techniques to secure the airway, such as endotracheal intubation or the use of supraglottic airway devices. Precise control over ventilation parameters is maintained to support oxygenation and prevent respiratory complications.
Intraoperative Awareness and Depth of Anesthesia
Avoiding intraoperative awareness (patient consciousness during surgery) is a priority in anesthesia management. Anesthesiologists carefully monitor the depth of anesthesia, utilizing advanced monitoring tools and clinical expertise. This diligence prevents patients from experiencing awareness while ensuring they remain comfortably sedated throughout the procedure.
Pain Management and Analgesia
Beyond sedation, anesthesia management includes effective pain management. Anesthesiologists administer analgesics to control postoperative pain and enhance the patient’s recovery experience. Balancing adequate pain relief with minimizing side effects is a delicate aspect of anesthesia management that requires both medical knowledge and empathy.
Preventing and Managing Complications
Anesthesia management encompasses a proactive approach to preventing and managing complications. Anesthesiologists are trained to identify potential issues before they escalate. In the rare event of complications, swift and decisive action is taken to address them promptly, ensuring patient safety and well-being.
Communication with the Surgical Team
Clear and effective communication is vital in anesthesia management. Anesthesiologists collaborate closely with the surgical team to coordinate the timing of anesthesia induction, ensure proper patient positioning, and align sedation levels with the procedural requirements. This teamwork contributes to the seamless flow of the entire medical intervention.
Postoperative Care and Recovery
Anesthesia management extends into the postoperative phase. Anesthesiologists oversee the transition from sedation to wakefulness, closely monitoring patients in the recovery room. This phase involves managing any lingering effects of anesthesia, ensuring pain control, and addressing any emerging issues as patients regain
Aligning Wellness: The Essence of Chiropractic Treatment

Aligning Wellness: Exploring the Essence of Chiropractic Treatment
Chiropractic treatment stands as a holistic approach to healthcare, focusing on the intricate connection between the spine and overall well-being. In this article, we delve into the principles of chiropractic care, the diverse treatments it offers, and the potential benefits for individuals seeking natural and non-invasive health solutions.
The Core Principles of Chiropractic Care
At the heart of chiropractic treatment lies the belief that proper alignment of the spine is essential for optimal health. Chiropractors emphasize the relationship between the musculoskeletal system and the nervous system, acknowledging the spine’s crucial role in facilitating communication between the body and the brain. Through manual adjustments, chiropractors aim to restore spinal alignment and promote the body’s innate ability to heal itself.
Manual Adjustments: Restoring Spinal Harmony
Central to chiropractic treatment are manual adjustments, also known as spinal manipulations. Chiropractors use controlled and precise force to manipulate the spine’s joints, aiming to correct misalignments or subluxations. This hands-on approach is designed to alleviate pain, improve joint mobility, and enhance the nervous system’s function. Manual adjustments form the foundation of chiropractic care, addressing issues ranging from back pain to headaches.
Addressing Musculoskeletal Conditions
Chiropractic treatment extends beyond spinal adjustments to address a wide array of musculoskeletal conditions. Chiropractors employ various therapeutic techniques, including soft tissue massage, stretching, and exercises, to alleviate tension, improve flexibility, and enhance overall musculoskeletal function. This comprehensive approach aims to address the root causes of discomfort and promote long-term musculoskeletal health.
Holistic Health and Wellness
Chiropractic care is inherently holistic, recognizing that the body functions as an integrated whole. Beyond symptom relief, chiropractors consider factors such as nutrition, lifestyle, and stress management in developing personalized treatment plans. This holistic approach aligns with the philosophy of treating the individual, not just the symptoms, fostering overall health and wellness.
Pain Management without Medication
One distinctive aspect of chiropractic treatment is its emphasis on drug-free pain management. Chiropractors utilize natural and non-invasive methods to alleviate pain, making it an appealing option for individuals seeking alternatives to medication. This approach aligns with the growing interest in holistic and integrative healthcare solutions that prioritize minimizing reliance on pharmaceutical interventions.
Chiropractic Care for Postural Correction
Modern lifestyles often contribute to poor posture, leading to a range of musculoskeletal issues. Chiropractic treatment addresses postural concerns by identifying and correcting misalignments that contribute to poor posture. Through targeted adjustments and exercises, chiropractors work to restore proper alignment, relieving strain on the spine and supporting improved posture.
Sports Injuries and Performance Optimization
Chiropractic care is increasingly sought after by athletes for injury prevention, rehabilitation, and performance optimization. Chiropractors employ specialized techniques to address sports-related injuries, enhance joint mobility, and improve overall athletic performance. The focus on biomechanics and functional movement aligns with athletes’ goals of staying active and achieving peak physical condition.
Tailored Care for Individual Needs
Chiropractic treatment is not a one-size-fits-all approach; instead, it is tailored to individual needs and health goals. Chiropractors conduct thorough assessments, considering factors such as
Elevating Care: Anesthesia Support Excellence

Catalysts of Comfort: Navigating Excellence in Anesthesia Support
In the realm of healthcare, the role of anesthesia support is paramount, ensuring that patients undergo medical procedures with safety, comfort, and precision. Anesthesia support professionals, including anesthesiologists and nurse anesthetists, play a crucial role in optimizing the patient experience and facilitating successful medical interventions. Let’s explore the multifaceted dimensions of anesthesia support and its pivotal role in healthcare settings.
The Foundation of Patient Safety
Anesthesia support serves as the bedrock of patient safety during medical procedures. Professionals in this field are dedicated to assessing the patient’s medical history, monitoring vital signs, and tailoring anesthesia plans to the individual’s unique needs. The focus on meticulous planning and continuous monitoring contributes to a safe and controlled environment for various surgical and medical interventions.
Tailored Anesthesia Plans for Diverse Procedures
Anesthesia support extends its expertise across a spectrum of medical procedures, ranging from routine surgeries to complex interventions. Professionals collaborate with surgical teams to devise tailored anesthesia plans that align with the specific requirements of each procedure. This personalized approach ensures that patients receive the appropriate type and dosage of anesthesia for their condition and the nature of the intervention.
Pain Management Expertise
Beyond inducing a state of controlled unconsciousness during surgery, anesthesia support is integral to pain management. Professionals work closely with patients to address preoperative anxiety and administer anesthesia that not only ensures unconsciousness but also manages postoperative pain effectively. This dual focus on patient comfort and pain control contributes to a smoother recovery process.
Navigating Anesthesia Techniques
Anesthesia support encompasses a repertoire of techniques, each designed to address different medical scenarios. From general anesthesia, where patients are completely unconscious, to regional anesthesia, which targets specific areas of the body, professionals navigate diverse techniques based on the nature of the procedure and the patient’s medical condition. This versatility allows for flexibility and precision in anesthesia administration.
Continuous Monitoring During Procedures
Throughout medical procedures, anesthesia support professionals maintain vigilant monitoring of vital signs, ensuring the patient’s physiological stability. From heart rate and blood pressure to oxygen saturation levels, continuous assessment allows for prompt interventions if any deviations from the norm occur. This real-time monitoring contributes to the overall safety and well-being of the patient.
Emergency Preparedness and Rapid Response
Anesthesia support professionals undergo extensive training in emergency preparedness and rapid response. While complications during anesthesia are rare, being prepared for any unforeseen circumstances is crucial. Professionals are equipped to handle emergencies swiftly, whether it involves allergic reactions, changes in vital signs, or other unexpected events, ensuring that patient safety remains the top priority.
Collaboration with Surgical Teams
Anesthesia support is a collaborative endeavor that involves close coordination with surgical teams. Effective communication between anesthesiologists, surgeons, and other healthcare professionals is essential for a seamless and successful medical intervention. This collaborative approach ensures that the patient’s overall well-being is prioritized throughout the entire perioperative period.
Postoperative Care and Recovery Support
The responsibilities of anesthesia support extend into the postoperative phase, encompassing care and support
Optimizing Wellness: Chiropractic Care Plans
Optimizing Wellness: Chiropractic Care Plans
Chiropractic care is more than just a treatment for back pain; it’s a holistic approach to wellness. Chiropractic care plans are designed to optimize overall health, addressing not only pain but also promoting balance and well-being. Let’s delve into the key elements of chiropractic care plans and their transformative impact on holistic health.
Understanding Chiropractic Care: Beyond Pain Relief
Chiropractic care focuses on the relationship between the spine and the nervous system, recognizing the spine’s role in overall health. While pain relief is a common reason for seeking chiropractic care, the approach goes beyond symptom management. Chiropractors aim to enhance the body’s natural ability to heal and function optimally.
Initial Assessment: Personalized Care Begins
The foundation of any chiropractic care plan is a thorough initial assessment. Chiropractors conduct a comprehensive examination, including a health history review, spinal evaluation, and, if necessary, diagnostic imaging. This personalized approach allows chiropractors to understand the individual’s unique needs and tailor a care plan accordingly.
Spinal Adjustments: Restoring Alignment
Central to chiropractic care are spinal adjustments, also known as spinal manipulations. Chiropractors use precise and controlled force to restore proper alignment of the spine. This not only alleviates pain and discomfort but also facilitates improved nerve function, promoting overall wellness.
Holistic Approach: Addressing the Whole Person
Chiropractic care plans take a holistic approach, addressing the whole person rather than isolated symptoms. Chiropractors consider factors such as lifestyle, nutrition, and stress management in developing a comprehensive plan that supports the body’s natural healing mechanisms.
Corrective Exercises: Empowering Patients
Chiropractic care extends beyond the clinic with the incorporation of corrective exercises. Chiropractors prescribe specific exercises to strengthen muscles, improve flexibility, and support the adjustments made during sessions. Empowering patients with exercises promotes long-term benefits and self-care.
Nutritional Guidance: Nourishing the Body
Nutritional guidance is often integrated into chiropractic care plans. Chiropractors recognize the impact of nutrition on overall health and may provide recommendations to support the body’s healing processes. A well-nourished body is better equipped to respond positively to chiropractic adjustments.
Wellness Education: Informing and Empowering
Education is a fundamental component of chiropractic care plans. Chiropractors educate patients about their spine, nervous system, and the importance of proactive wellness. Informed patients are empowered to make lifestyle choices that contribute to long-term health and prevent future issues.
Progress Monitoring: Adapting Care Plans
Chiropractic care is dynamic, and care plans are adapted based on the individual’s progress. Regular reassessment allows chiropractors to monitor improvements, adjust techniques if needed, and ensure the ongoing effectiveness of the care plan.
Pain Management and Prevention: Dual Focus
While chiropractic care is effective in managing pain, its emphasis on prevention sets it apart. Chiropractors work with patients to identify and address underlying issues, reducing the likelihood of recurring pain and promoting sustained well-being.
Accessing Chiropractic Care Plans
For those seeking a holistic approach to health and wellness, Chiropractic Care Plans offers valuable insights. Explore the transformative possibilities of chiropractic care plans in optimizing well-being and fostering a balanced, pain-free
Navigating Anesthesia: Innovative Approaches for Comfort

Exploring the Frontiers of Comfort: Innovative Anesthesia Approaches
The realm of anesthesia has witnessed significant advancements over the years, revolutionizing the way patients experience medical procedures. From traditional methods to cutting-edge approaches, the field has embraced innovations that prioritize both efficacy and patient comfort. Let’s delve into the world of anesthesia approaches, understanding how they contribute to a more seamless and comfortable medical experience.
Evolution of Anesthesia Techniques
Anesthesia has come a long way since its inception, evolving from simple herbal concoctions to sophisticated pharmaceutical agents. Today, anesthetic approaches are tailored to meet the specific needs of patients and the requirements of diverse medical procedures. The evolution of anesthesia techniques reflects a commitment to enhancing patient safety and comfort.
Regional Anesthesia: Targeting Specific Areas
One notable innovation in anesthesia approaches is the emphasis on regional anesthesia. This technique involves numbing a specific part of the body, allowing patients to undergo surgery or medical procedures while remaining conscious. Common forms of regional anesthesia include epidurals for childbirth and peripheral nerve blocks for orthopedic surgeries. These approaches minimize the need for general anesthesia and contribute to faster recovery times.
Balancing Sedation: Twilight Anesthesia
Twilight anesthesia, also known as conscious sedation, occupies a middle ground between local and general anesthesia. It induces a state of deep relaxation and drowsiness while allowing patients to maintain a level of consciousness. This approach is often employed for less invasive procedures, such as dental work or endoscopies, providing a comfortable experience without the complete loss of consciousness associated with general anesthesia.
Patient-Centric Care: Tailored Anesthetic Plans
Modern anesthesia approaches prioritize patient-centric care by tailoring anesthetic plans to individual needs. Anesthesiologists work closely with patients to understand their medical history, preferences, and any concerns they may have. This collaborative approach ensures that the chosen anesthesia method aligns with the patient’s comfort level and contributes to a positive overall experience.
Enhanced Recovery After Surgery (ERAS): Optimizing Outcomes
Anesthesia approaches play a pivotal role in Enhanced Recovery After Surgery (ERAS) protocols. By employing multimodal anesthesia techniques, including regional anesthesia and targeted pain management, ERAS aims to minimize the physiological stress of surgery and accelerate postoperative recovery. These innovative approaches not only enhance patient comfort but also contribute to shorter hospital stays and improved outcomes.
Technological Integration: Smart Anesthesia
Advancements in technology have led to the integration of smart systems in anesthesia administration. Automated anesthesia delivery systems, combined with monitoring technologies, enable precise control over the depth of anesthesia. This technological synergy ensures a more accurate and individualized administration of anesthesia, enhancing patient safety and optimizing the overall anesthesia experience.
Pediatric-Focused Approaches: Comfort for the Little Ones
Anesthesia approaches for pediatric patients require special considerations. Pediatric anesthesiologists employ techniques that prioritize safety and comfort for children undergoing surgeries or medical procedures. Tailored approaches, such as inhalation anesthesia or pediatric regional blocks, contribute to a positive experience for young patients and their families.
Pain Management Innovations: Beyond the Procedure
Anesthesia approaches extend beyond the surgical or procedural phase to encompass postoperative pain
Elevating Wellness: Expert Chiropractic Care

Elevating Wellness: Expert Chiropractic Care
Chiropractic expertise plays a pivotal role in promoting overall well-being by focusing on the spine’s alignment and its impact on the nervous system. In this article, we’ll delve into the importance of expert chiropractic care, exploring the principles, benefits, and the positive influence it can have on one’s health.
Understanding Chiropractic Principles
Chiropractic care is grounded in the principle that the spine’s alignment directly influences the nervous system. The spine houses the spinal cord, a crucial component of the nervous system responsible for transmitting signals between the brain and the rest of the body. Expert chiropractors understand the intricate relationship between spinal health and overall well-being.
Holistic Approach to Health and Healing
Chiropractic expertise embraces a holistic approach to health and healing. Rather than merely addressing symptoms, chiropractors focus on the root cause of health issues, often related to spinal misalignments. By restoring proper spinal alignment, chiropractic care seeks to optimize the body’s ability to heal itself, promoting long-term wellness.
Spinal Adjustments: Restoring Balance
Central to chiropractic expertise are spinal adjustments. These manual manipulations aim to restore the spine’s natural alignment, addressing issues such as subluxations and misalignments. This process enhances nerve function, reduces inflammation, and contributes to improved overall health and mobility.
Nervous System Optimization
Chiropractic care is intricately connected to optimizing the nervous system. When the spine is misaligned, it can exert pressure on nerves, leading to disruptions in communication between the brain and the body. Expert chiropractors employ precise adjustments to alleviate this pressure, facilitating optimal nervous system function.
Pain Management and Injury Prevention
Chiropractic care is renowned for its effectiveness in pain management and injury prevention. By addressing the root causes of pain, rather than merely masking symptoms, chiropractors offer natural and non-invasive solutions. This approach is especially valuable for conditions like back pain, neck pain, and headaches.
Enhancing Mobility and Range of Motion
Expert chiropractic care contributes to enhanced mobility and increased range of motion. Through targeted adjustments, chiropractors address restrictions in joint movement, promoting flexibility and reducing stiffness. This is particularly beneficial for individuals dealing with musculoskeletal issues or those looking to improve athletic performance.
Individualized Treatment Plans
Chiropractic expertise recognizes that each individual is unique, and one-size-fits-all approaches may not be effective. Expert chiropractors tailor treatment plans to address specific health needs and goals. This personalized approach ensures that individuals receive the most effective and targeted care for their well-being.
Collaboration with Other Healthcare Professionals
Chiropractors often collaborate with other healthcare professionals to provide comprehensive care. This interdisciplinary approach ensures that patients receive well-rounded treatment and addresses various aspects of their health. Communication between chiropractors and other healthcare providers enhances the overall effectiveness of patient care.
Educating Patients for Long-Term Wellness
An integral aspect of chiropractic expertise is patient education. Chiropractors empower patients with knowledge about their spinal health, lifestyle choices, and exercises to support long-term wellness. Educated patients are better equipped to make informed decisions that contribute to their overall health and well-being.
Explore Chiropractic Expertise at
Ensuring Comfort: Excellence in Anesthesia Care

Ensuring Comfort: Excellence in Anesthesia Care
Anesthesia care plays a pivotal role in medical procedures, ensuring patients’ comfort and safety. This specialized field involves highly skilled professionals who administer anesthesia, monitor patients throughout surgeries, and manage pain during the recovery process. Let’s explore the crucial aspects of anesthesia care and its significance in modern healthcare.
The Fundamental Role of Anesthesia in Medical Procedures
Anesthesia is a critical component of various medical procedures, ranging from minor surgeries to complex interventions. It serves the purpose of inducing a reversible loss of sensation, allowing surgeons to perform procedures without causing pain or discomfort to the patient. Anesthesia care is tailored to each individual, considering their medical history, procedure type, and overall health.
Types of Anesthesia: Tailoring Care to Individual Needs
Anesthesia care encompasses different types tailored to the specific needs of patients and procedures. General anesthesia induces a state of unconsciousness, regional anesthesia targets a specific part of the body, and local anesthesia numbs a small area. The choice depends on the nature of the surgery and the patient’s health conditions, emphasizing the importance of personalized care.
The Anesthesiologist’s Expertise: Ensuring Patient Safety
Anesthesiologists, medical doctors specialized in anesthesia, lead the anesthesia care team. Their expertise goes beyond administering anesthesia; they conduct preoperative assessments, develop anesthetic plans, monitor vital signs during surgery, and manage pain postoperatively. The presence of an anesthesiologist ensures a comprehensive approach to patient safety and comfort.
Precision Monitoring Throughout Surgery
Anesthesia care involves continuous monitoring of the patient’s vital signs throughout the surgical procedure. This includes heart rate, blood pressure, oxygen levels, and more. Anesthesiologists and anesthesia providers closely track these parameters to respond promptly to any changes, ensuring the patient’s well-being and maintaining a stable physiological state.
Pain Management in Postoperative Recovery
Beyond the operating room, anesthesia care extends into postoperative recovery. Anesthesia providers play a crucial role in managing pain and discomfort as patients awaken from surgery. Tailored pain management plans may include medications, nerve blocks, or other techniques to enhance recovery and improve the overall postoperative experience.
Collaborative Approach in Anesthesia Care
Anesthesia care is inherently collaborative. Anesthesiologists work closely with surgeons, nurses, and other healthcare professionals to create a seamless and safe perioperative experience. Effective communication and coordination among the healthcare team members contribute to successful outcomes and patient satisfaction.
Innovations in Anesthesia Techniques
Advancements in medical technology and anesthesia techniques continue to enhance patient care. Targeted drug delivery systems, enhanced monitoring devices, and improved pain management protocols are among the innovations that contribute to the evolution of anesthesia care. These innovations aim to make procedures safer, more efficient, and more comfortable for patients.
Patient Education and Informed Consent
Anesthesia care includes a crucial component of patient education and obtaining informed consent. Anesthesiologists discuss the planned anesthesia approach, potential risks, and expected outcomes with patients before the procedure. This ensures that patients are well-informed, actively involved in their care decisions, and have realistic expectations about their anesthesia experience.
Ensuring Accessible and Inclusive Care
In the
Revitalizing Health: Comprehensive Chiropractic Services

Revitalizing Health: Comprehensive Chiropractic Services
Chiropractic services offer a holistic approach to health, focusing on the relationship between the spine and overall well-being. In this article, we’ll explore the various aspects of chiropractic care and how it contributes to revitalizing health and promoting a balanced lifestyle.
Understanding Chiropractic Philosophy
Chiropractic care is grounded in the belief that the spine’s alignment directly influences the body’s function. By addressing misalignments, known as subluxations, chiropractors aim to enhance the body’s natural ability to heal and maintain optimal health. This philosophy forms the basis for comprehensive chiropractic services.
Spinal Adjustments: Restoring Alignment and Function
Central to chiropractic care are spinal adjustments, where chiropractors use precise and controlled force to realign the spine. These adjustments not only alleviate pain but also enhance nervous system function, promoting better communication between the brain and the rest of the body. Restoring proper alignment is key to revitalizing health.
Pain Management and Beyond
While chiropractic care is often sought for pain relief, its benefits extend beyond addressing discomfort. Chiropractors evaluate the root cause of pain and work towards long-term solutions. This proactive approach not only manages pain but contributes to overall well-being, fostering a healthier and more balanced lifestyle.
Chiropractic Care for Improved Mobility
The spine’s alignment directly influences joint mobility. Chiropractic services focus on enhancing range of motion, addressing stiffness, and promoting flexibility. By optimizing spinal function, individuals experience improved mobility, making daily activities more comfortable and enjoyable.
Holistic Wellness: Beyond Symptom Relief
Chiropractic care emphasizes holistic wellness, acknowledging the interconnectedness of various bodily systems. Beyond symptom relief, chiropractors work with patients to enhance overall health, considering factors such as nutrition, exercise, and lifestyle choices. This comprehensive approach fosters a proactive stance towards well-being.
Preventive Chiropractic Services
Preventive care is a cornerstone of chiropractic services. Regular check-ups and adjustments help identify and address potential issues before they escalate. This proactive approach aligns with the philosophy of maintaining optimal health and preventing future discomfort or dysfunction.
Chiropractic Care for Stress Reduction
The impact of spinal misalignments on the nervous system can contribute to heightened stress levels. Chiropractic adjustments help reduce stress by promoting relaxation and restoring balance to the nervous system. This holistic approach to stress management contributes to overall mental and physical well-being.
Sports Performance and Chiropractic Care
Athletes often turn to chiropractic care to enhance sports performance. By optimizing spinal alignment, athletes experience improved biomechanics, reduced risk of injuries, and enhanced recovery. Chiropractic services play a crucial role in supporting athletes in achieving their peak performance levels.
Chiropractic Care for Every Age Group
Chiropractic care is not limited to specific age groups; it benefits individuals from childhood to senior years. Pediatric chiropractic care addresses developmental concerns, while chiropractic adjustments for seniors focus on mobility and pain management. This inclusivity highlights the adaptability and effectiveness of chiropractic services across the lifespan.
Explore the Benefits of Chiropractic Services
To explore the diverse benefits of chiropractic services and how they can contribute to your well-being, visit Chiropractic Services. Discover
Holistic Healing: Chiropractic Care for Optimal Wellness

Unlocking Holistic Wellness: The Essence of Chiropractic Care
Chiropractic care has emerged as a holistic approach to wellness, emphasizing the intricate connection between the spine, nervous system, and overall health. In this exploration of chiropractic care, we delve into its principles, benefits, and the role it plays in fostering optimal well-being.
The Foundation: Understanding Chiropractic Principles
At the core of chiropractic care is the belief that the spine’s alignment directly influences the nervous system, impacting various bodily functions. Chiropractors focus on the spine’s adjustment, aiming to correct misalignments, known as subluxations, to restore balance and facilitate the body’s natural healing processes.
Beyond Symptom Relief: Chiropractic’s Holistic Approach
Unlike traditional medicine, chiropractic care goes beyond symptom relief. Rather than merely addressing symptoms, chiropractors seek to identify and correct the root causes of health issues. By enhancing the body’s innate ability to heal, chiropractic care embraces a holistic approach to well-being.
Benefits of Chiropractic Care for Pain Management
One of the most well-known aspects of chiropractic care is its effectiveness in managing pain, particularly in the spine and musculoskeletal system. Through spinal adjustments and manipulations, chiropractors can alleviate discomfort, enhance joint mobility, and promote overall pain relief without relying on medications.
Improving Functionality: Chiropractic Care and Joint Health
Chiropractic care extends its benefits beyond pain relief, emphasizing the improvement of joint functionality. By addressing misalignments, chiropractors contribute to better joint mobility and function. This, in turn, supports a more active lifestyle and reduces the risk of injuries related to joint issues.
Enhancing Nervous System Function: The Backbone of Health
The spine’s alignment directly influences the nervous system, which controls and coordinates bodily functions. Chiropractic care aims to optimize nervous system function by ensuring a well-aligned spine. This can lead to improvements in overall health, immune system response, and the body’s ability to adapt to stress.
Chiropractic Care for Posture Correction
In the modern era of sedentary lifestyles and prolonged screen time, poor posture has become a common concern. Chiropractic care offers corrective measures to address postural issues, promoting better spinal alignment. Improved posture not only alleviates discomfort but also contributes to enhanced overall well-being.
Holistic Wellness for Every Age: Pediatric and Geriatric Chiropractic Care
Chiropractic care is adaptable to individuals of all ages. Pediatric chiropractic care focuses on ensuring healthy development and addressing potential issues early in life. In the geriatric population, chiropractic care contributes to maintaining mobility, managing age-related conditions, and promoting overall vitality.
Chiropractic Care and Stress Reduction
Stress has a profound impact on health, contributing to various physical and mental issues. Chiropractic care recognizes the interconnectedness of the spine and nervous system with stress levels. Through spinal adjustments, chiropractors aim to reduce tension, promote relaxation, and contribute to overall stress reduction.
The Role of Chiropractic Care in Preventive Health
Beyond addressing existing health concerns, chiropractic care plays a crucial role in preventive health. Regular chiropractic adjustments can help identify and correct potential issues before they manifest as symptoms. This proactive approach aligns with the philosophy of holistic well-being and
Optimizing Anesthesia Management for Surgical Excellence
Optimizing Anesthesia Management for Surgical Excellence
Effective anesthesia management is a critical component of ensuring successful surgical outcomes. From preoperative assessments to postoperative care, a comprehensive approach to anesthesia contributes significantly to patient safety and overall surgical success.
The Importance of Personalized Anesthesia Plans
Every patient is unique, and their medical history, allergies, and overall health condition must be carefully considered when formulating an anesthesia plan. Personalized anesthesia plans not only enhance patient safety but also contribute to improved recovery times and overall satisfaction.
Advanced Technologies in Anesthesia Delivery
In recent years, technological advancements have revolutionized anesthesia delivery. From precision-controlled anesthesia machines to advanced monitoring devices, these technologies enable anesthesiologists to tailor the administration of anesthesia to each patient’s specific needs. The integration of technology ensures a more accurate and controlled anesthesia experience.
Collaboration between Anesthesiologists and Surgical Teams
Effective communication and collaboration between anesthesiologists and surgical teams are paramount. Anesthesiologists work closely with surgeons to understand the intricacies of each procedure, ensuring the administration of the appropriate type and level of anesthesia. This collaboration enhances overall surgical efficiency and patient care.
Preoperative Assessments: A Key to Safe Anesthesia
Thorough preoperative assessments are crucial in identifying any potential risks or complications associated with anesthesia. Patient history, physical examinations, and diagnostic tests help anesthesiologists make informed decisions, ensuring that the chosen anesthesia approach aligns with the patient’s health status and the requirements of the surgery.
Patient Education and Informed Consent
Educating patients about the anesthesia process and obtaining informed consent are essential steps in promoting a positive surgical experience. Patients should be aware of what to expect, potential side effects, and the importance of providing accurate medical information to the anesthesia team. Informed patients are better equipped to actively participate in their care.
Monitoring During Surgery for Optimal Anesthesia Management
Continuous monitoring during surgery is critical for adjusting anesthesia levels and responding promptly to any changes in the patient’s condition. Advanced monitoring equipment allows anesthesiologists to track vital signs, ensuring a delicate balance between maintaining anesthesia depth and safeguarding patient well-being.
Postoperative Care and Pain Management
Anesthesia management extends into the postoperative period, where anesthesiologists play a role in pain management strategies. Tailored pain management plans contribute to a smoother recovery process, minimizing discomfort and facilitating the patient’s transition from the operating room to the recovery phase.
Continuous Professional Development for Anesthesia Teams
Staying abreast of the latest developments in anesthesia is essential for anesthesia teams. Continuous professional development ensures that anesthesiologists and supporting staff are well-informed about emerging techniques, technologies, and best practices, ultimately enhancing the quality of anesthesia care provided.
Anesthesia Management: A Link to Successful Surgeries
In the pursuit of surgical excellence, the role of anesthesia management cannot be overstated. It is a dynamic field where precision, collaboration, and ongoing education converge to ensure the highest standards of patient care. Explore more about the nuances of Anesthesia Management at Anesthesia Management for valuable insights and resources to support optimal surgical outcomes.
In conclusion, optimizing anesthesia management involves a
Anesthesia Harmony: Optimal Care for Comfort

Anesthesia Harmony: Optimal Care for Comfort
Anesthesia care is a critical component of medical procedures, ensuring patients experience optimal comfort and safety throughout their healthcare journey. From pre-operative assessments to post-anesthesia monitoring, the seamless orchestration of anesthesia care contributes significantly to positive surgical outcomes and patient well-being.
Pre-Operative Assessment: Tailoring Anesthesia Plans
The journey of anesthesia care begins with a thorough pre-operative assessment. Anesthesiologists carefully evaluate patients’ medical history, current health status, and any existing conditions to tailor anesthesia plans accordingly. This personalized approach ensures that the chosen anesthesia technique aligns with the individual’s needs, optimizing the overall care experience.
Patient Education: Fostering Informed Consent
A key aspect of anesthesia care is patient education. Anesthesiologists take the time to explain the chosen anesthesia method, potential side effects, and what to expect during the procedure. This communication fosters informed consent, empowering patients with knowledge and alleviating concerns about the anesthesia process. A well-informed patient is better positioned to actively participate in their care journey.
Intraoperative Management: Ensuring Anesthesia Efficacy
During the actual procedure, the expertise of anesthesiologists shines in the realm of intraoperative management. They carefully administer and monitor anesthesia to ensure its efficacy and safety. Constant vigilance allows for adjustments in dosage or technique, responding to the dynamic nature of surgery and promoting a stable and comfortable intraoperative experience for the patient.
Pain Management: Precision in Analgesia
Anesthesia care extends to effective pain management, both during and after surgery. Anesthesiologists employ precise techniques to control pain, utilizing a combination of general anesthesia, regional anesthesia, or analgesic medications. The goal is to minimize discomfort, enhance recovery, and contribute to an overall positive postoperative experience for the patient.
Post-Anesthesia Care: Monitoring Recovery
The continuum of anesthesia care extends into the post-anesthesia care unit (PACU), where vigilant monitoring ensures a smooth transition from the effects of anesthesia to wakefulness. Anesthesiologists and specialized nurses closely observe patients, addressing any emerging concerns promptly. This phase is crucial in managing the initial stages of recovery and providing immediate support if needed.
Regional Anesthesia: Targeted Pain Relief
In certain cases, regional anesthesia becomes a focal point of anesthesia care. Techniques such as epidurals or nerve blocks target specific regions of the body, providing targeted pain relief without rendering the patient fully unconscious. Regional anesthesia plays a vital role in pain management for various surgical procedures, contributing to a more nuanced and tailored approach.
Pediatric Anesthesia: Tailoring Care for Young Patients
Anesthesia care extends its expertise to pediatric patients, requiring a specialized approach. Pediatric anesthesiologists are adept at tailoring care to the unique needs of children, considering factors such as age, weight, and developmental stage. Their focus is on ensuring safety, comfort, and a positive experience for the young patients undergoing medical procedures.
Collaboration with Surgical Teams: Synergy for Success
The success of anesthesia care is closely intertwined with collaboration among healthcare professionals. Anesthesiologists work in synergy with surgical teams, communicating effectively to coordinate the timing and delivery of anesthesia. This collaborative approach ensures that anesthesia seamlessly aligns

