Continuous Professional Development
Radiology Mastery: Expertise in Medical Imaging

Radiology Mastery: Expertise in Medical Imaging
Radiology expertise is a cornerstone of modern healthcare, playing a crucial role in diagnostic accuracy, treatment planning, and patient care. From interpreting complex images to staying abreast of technological advancements, radiologists with expertise in medical imaging contribute significantly to the effectiveness and precision of healthcare practices.
Interpreting Complex Images: The Art of Diagnosis
At the heart of radiology expertise lies the ability to interpret complex medical images. Radiologists undergo rigorous training to decipher X-rays, CT scans, MRIs, and other imaging modalities. Their keen eye and specialized knowledge enable them to identify abnormalities, diagnose conditions, and provide crucial information that guides medical decision-making.
Utilizing Advanced Imaging Technologies: Staying at the Forefront
Radiology expertise extends to the utilization of advanced imaging technologies. Staying at the forefront of technological advancements, radiologists leverage tools such as 3D imaging, artificial intelligence, and molecular imaging. This integration of cutting-edge technologies enhances diagnostic capabilities, allowing for more accurate and nuanced assessments.
Specialized Knowledge for Various Medical Fields: Tailored Insights
Radiologists with expertise bring specialized knowledge to various medical fields. Whether in oncology, neurology, cardiology, or musculoskeletal imaging, their understanding of the unique aspects of each specialty ensures tailored insights. This specialization is instrumental in providing detailed and relevant information crucial for precise diagnoses and treatment planning.
Collaboration with Healthcare Teams: A Multidisciplinary Approach
Radiology expertise thrives on collaboration with healthcare teams. Radiologists work closely with physicians, surgeons, and other specialists to contribute their imaging insights to the overall patient care plan. This multidisciplinary approach ensures that medical decisions are well-informed, comprehensive, and aligned with the best interests of the patient.
Quality Assurance: Ensuring Accurate and Reliable Results
In the realm of radiology, expertise includes a commitment to quality assurance. Radiologists employ rigorous protocols to ensure the accuracy and reliability of imaging results. From image acquisition to interpretation, every step is carefully monitored to maintain the highest standards, contributing to the overall integrity of the diagnostic process.
Continuous Learning and Professional Development: Staying Updated
Radiologists with expertise embrace a culture of continuous learning and professional development. The field of medical imaging evolves rapidly, with new technologies and research emerging regularly. By staying updated, radiologists ensure that their expertise remains relevant and that they can effectively navigate the dynamic landscape of radiology.
Patient-Centric Communication: Translating Findings Effectively
Expertise in radiology goes beyond technical proficiency; it includes patient-centric communication. Radiologists with expertise have the ability to translate complex findings into understandable language for patients and referring physicians. Clear communication is vital for ensuring that patients comprehend their diagnoses and treatment options, fostering a collaborative approach to healthcare.
Research and Innovation: Contributing to Advancements
Radiology expertise often involves engagement in research and innovation. Radiologists may participate in clinical trials, explore new imaging techniques, and contribute to scientific advancements in the field. This commitment to research enhances the overall body of knowledge in radiology and propels the field forward, benefiting patient care on a broader scale.
Explore the Impact of Radiology Expertise
To delve deeper into
Decoding Images: Expert Radiology Interpretation for Precision

Decoding Images: The Art and Science of Radiology Interpretation
Radiology interpretation is a crucial aspect of modern healthcare, bridging the gap between medical imaging and diagnostic insights. This intricate process involves highly trained professionals who play a pivotal role in deciphering complex images to provide precise diagnoses and inform effective treatment plans.
The Expertise Behind Radiology Interpretation
Radiology interpretation requires a unique set of skills and expertise. Radiologists, specialized physicians in this field, undergo extensive training to develop a keen understanding of anatomy, pathology, and the nuances of various imaging modalities. Their expertise is instrumental in accurately interpreting medical images for a diverse range of conditions.
Navigating the World of Medical Imaging
The realm of medical imaging is vast, encompassing techniques such as X-rays, computed tomography (CT), magnetic resonance imaging (MRI), ultrasound, and more. Each modality provides distinct views of the body, and radiologists must navigate through this plethora of images to derive meaningful information. Radiology interpretation transforms visual data into actionable insights.
Precision in Diagnoses through Radiology Interpretation
The primary goal of radiology interpretation is to achieve precision in diagnoses. Whether identifying fractures in an X-ray, visualizing internal organs in an MRI, or detecting abnormalities in a CT scan, radiologists meticulously analyze images to unveil subtle details that may indicate various medical conditions. This precision is crucial for guiding appropriate medical interventions.
Multidisciplinary Collaboration for Comprehensive Insights
Radiology interpretation often involves collaboration with other medical specialists, fostering a multidisciplinary approach to patient care. Radiologists work closely with referring physicians, surgeons, and other healthcare professionals to ensure comprehensive insights into a patient’s condition. This collaborative effort enhances the accuracy and effectiveness of medical decision-making.
Advanced Technologies Shaping Radiology Interpretation
Technological advancements continually shape the landscape of radiology interpretation. Artificial intelligence (AI) applications, for instance, assist radiologists in image analysis, speeding up the process and providing additional layers of insight. While technology enhances efficiency, the human expertise of radiologists remains irreplaceable in nuanced interpretations.
Tailoring Interpretations to Individual Patient Needs
Radiology interpretation extends beyond identifying abnormalities; it involves tailoring interpretations to individual patient needs. Patient factors, medical history, and the specific clinical question at hand all influence how radiologists analyze images. This personalized approach ensures that interpretations contribute directly to the unique context of each patient’s healthcare journey.
Communication of Findings for Informed Decision-Making
Effective communication of radiology findings is a critical aspect of the interpretation process. Radiologists provide detailed reports to referring physicians, conveying their analyses and diagnostic impressions. Clear and timely communication is essential for informed decision-making, enabling healthcare teams to devise appropriate treatment plans for their patients.
Continuous Learning and Professional Development
The field of radiology is dynamic, with ongoing advancements in imaging technologies and medical knowledge. Radiologists engage in continuous learning and professional development to stay abreast of these changes. This commitment to lifelong learning ensures that radiologists remain at the forefront of their field, delivering the highest standard of care.
For more information on the art and science of Radiology Interpretation, visit www.dylanmessaging.com. Radiologists decode
Precision in Sedation: Anesthesia Management Mastery
Precision in Sedation: Anesthesia Management Mastery
Effective anesthesia management is a cornerstone of patient safety and comfort during medical procedures. In this article, we delve into the intricate world of anesthesia management, exploring the key components, safety measures, and the expertise required to ensure precision in sedation.
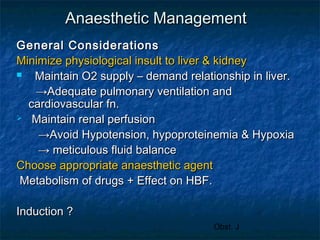
Patient Assessment and Individualized Plans
Anesthesia management begins with a thorough patient assessment. Anesthesiologists evaluate medical history, current health status, and any potential risks. Individualized anesthesia plans are then crafted, taking into account factors such as age, existing medical conditions, and the specific procedure requirements. This personalized approach enhances safety and optimizes sedation outcomes.
Selection and Administration of Anesthetic Agents
The choice and administration of anesthetic agents are critical aspects of anesthesia management. Anesthesiologists select the most suitable drugs based on the patient’s needs and the nature of the procedure. Precision in dosage and monitoring ensures that patients receive the right level of sedation while minimizing the risk of adverse effects.
Continuous Monitoring and Adjustments
During procedures, continuous monitoring is paramount. Anesthesia management involves vigilant tracking of vital signs, including heart rate, blood pressure, and oxygen levels. Anesthesiologists make real-time adjustments to the anesthesia delivery to maintain the desired level of sedation and respond promptly to any changes in the patient’s condition.
Airway Management and Ventilation
Ensuring a patent airway and proper ventilation is a fundamental responsibility in anesthesia management. Anesthesiologists employ various techniques to secure the airway, such as endotracheal intubation or the use of supraglottic airway devices. Precise control over ventilation parameters is maintained to support oxygenation and prevent respiratory complications.
Intraoperative Awareness and Depth of Anesthesia
Avoiding intraoperative awareness (patient consciousness during surgery) is a priority in anesthesia management. Anesthesiologists carefully monitor the depth of anesthesia, utilizing advanced monitoring tools and clinical expertise. This diligence prevents patients from experiencing awareness while ensuring they remain comfortably sedated throughout the procedure.
Pain Management and Analgesia
Beyond sedation, anesthesia management includes effective pain management. Anesthesiologists administer analgesics to control postoperative pain and enhance the patient’s recovery experience. Balancing adequate pain relief with minimizing side effects is a delicate aspect of anesthesia management that requires both medical knowledge and empathy.
Preventing and Managing Complications
Anesthesia management encompasses a proactive approach to preventing and managing complications. Anesthesiologists are trained to identify potential issues before they escalate. In the rare event of complications, swift and decisive action is taken to address them promptly, ensuring patient safety and well-being.
Communication with the Surgical Team
Clear and effective communication is vital in anesthesia management. Anesthesiologists collaborate closely with the surgical team to coordinate the timing of anesthesia induction, ensure proper patient positioning, and align sedation levels with the procedural requirements. This teamwork contributes to the seamless flow of the entire medical intervention.
Postoperative Care and Recovery
Anesthesia management extends into the postoperative phase. Anesthesiologists oversee the transition from sedation to wakefulness, closely monitoring patients in the recovery room. This phase involves managing any lingering effects of anesthesia, ensuring pain control, and addressing any emerging issues as patients regain
Elevating Care: Crucial Anesthesia Support

Elevating Care: The Vital Role of Anesthesia Support
The Backbone of Surgical Procedures: Anesthesia Support Unveiled
Anesthesia support plays a pivotal role in the realm of surgical procedures, serving as the backbone that ensures patients undergo interventions with safety, comfort, and precision. Behind the scenes, anesthesiologists and anesthesia teams collaborate seamlessly to administer anesthesia, monitor vital signs, and oversee the patient’s well-being throughout the entire surgical journey.
Anesthesiologists: Masters of Precision and Patient Safety
Anesthesiologists are the masters of precision in the operating room. Their expertise lies not only in administering the right dosage of anesthesia but also in tailoring it to the unique needs of each patient. With a keen focus on patient safety, anesthesiologists carefully assess medical histories, monitor vital signs, and make real-time adjustments to ensure a smooth and secure anesthesia experience.
Customizing Anesthesia Plans: Personalized Patient Care
One of the key aspects of anesthesia support is the customization of anesthesia plans. Anesthesiologists take into account various factors, including the type of surgery, the patient’s overall health, and any specific considerations or preferences. This personalized approach enhances the effectiveness of anesthesia while minimizing potential risks and ensuring the patient’s comfort.
Beyond General Anesthesia: Exploring Different Modalities
Anesthesia support extends beyond the realm of general anesthesia. Anesthesiologists are proficient in a variety of anesthesia modalities, including regional anesthesia and conscious sedation. These alternatives offer flexibility and allow for tailored approaches depending on the nature of the surgical procedure and the patient’s medical condition.
Monitoring Vital Signs: Ensuring Stability Throughout Surgery
Throughout surgery, anesthesia support involves vigilant monitoring of vital signs. Anesthesiologists continuously track factors such as heart rate, blood pressure, oxygen levels, and respiratory function. This real-time monitoring enables immediate intervention if any deviations from the norm occur, ensuring the patient remains stable and safe during the surgical process.
Patient Advocates in the Operating Room: Anesthesia Teams in Action
Anesthesia support is a collaborative effort involving not only anesthesiologists but also anesthesia teams. Nurse anesthetists and anesthesia assistants work alongside anesthesiologists, contributing their skills and expertise to guarantee a seamless and well-coordinated perioperative experience. This teamwork is fundamental in addressing the diverse needs of patients and surgical procedures.
Postoperative Care: Anesthesia’s Impact Beyond the Operating Room
The impact of anesthesia support extends beyond the operating room and into the postoperative period. Anesthesiologists play a crucial role in managing pain and ensuring a smooth transition to the recovery phase. Their involvement contributes to a positive recovery experience, aligning with the overall goal of enhancing patient outcomes and satisfaction.
Continuous Professional Development: Staying Ahead in Anesthesia Care
Anesthesia support is a dynamic field that undergoes constant advancements. Anesthesiologists and their teams engage in continuous professional development to stay abreast of the latest technologies, techniques, and safety protocols. This commitment to ongoing education reflects the dedication of anesthesia professionals to providing state-of-the-art care.
Patient Education and Communication: Fostering Trust and Understanding
Effective communication is an integral aspect of anesthesia support. Anesthesia teams prioritize patient education, ensuring individuals have a clear understanding
Optimizing Anesthesia Management for Surgical Excellence
Optimizing Anesthesia Management for Surgical Excellence
Effective anesthesia management is a critical component of ensuring successful surgical outcomes. From preoperative assessments to postoperative care, a comprehensive approach to anesthesia contributes significantly to patient safety and overall surgical success.
The Importance of Personalized Anesthesia Plans
Every patient is unique, and their medical history, allergies, and overall health condition must be carefully considered when formulating an anesthesia plan. Personalized anesthesia plans not only enhance patient safety but also contribute to improved recovery times and overall satisfaction.
Advanced Technologies in Anesthesia Delivery
In recent years, technological advancements have revolutionized anesthesia delivery. From precision-controlled anesthesia machines to advanced monitoring devices, these technologies enable anesthesiologists to tailor the administration of anesthesia to each patient’s specific needs. The integration of technology ensures a more accurate and controlled anesthesia experience.
Collaboration between Anesthesiologists and Surgical Teams
Effective communication and collaboration between anesthesiologists and surgical teams are paramount. Anesthesiologists work closely with surgeons to understand the intricacies of each procedure, ensuring the administration of the appropriate type and level of anesthesia. This collaboration enhances overall surgical efficiency and patient care.
Preoperative Assessments: A Key to Safe Anesthesia
Thorough preoperative assessments are crucial in identifying any potential risks or complications associated with anesthesia. Patient history, physical examinations, and diagnostic tests help anesthesiologists make informed decisions, ensuring that the chosen anesthesia approach aligns with the patient’s health status and the requirements of the surgery.
Patient Education and Informed Consent
Educating patients about the anesthesia process and obtaining informed consent are essential steps in promoting a positive surgical experience. Patients should be aware of what to expect, potential side effects, and the importance of providing accurate medical information to the anesthesia team. Informed patients are better equipped to actively participate in their care.
Monitoring During Surgery for Optimal Anesthesia Management
Continuous monitoring during surgery is critical for adjusting anesthesia levels and responding promptly to any changes in the patient’s condition. Advanced monitoring equipment allows anesthesiologists to track vital signs, ensuring a delicate balance between maintaining anesthesia depth and safeguarding patient well-being.
Postoperative Care and Pain Management
Anesthesia management extends into the postoperative period, where anesthesiologists play a role in pain management strategies. Tailored pain management plans contribute to a smoother recovery process, minimizing discomfort and facilitating the patient’s transition from the operating room to the recovery phase.
Continuous Professional Development for Anesthesia Teams
Staying abreast of the latest developments in anesthesia is essential for anesthesia teams. Continuous professional development ensures that anesthesiologists and supporting staff are well-informed about emerging techniques, technologies, and best practices, ultimately enhancing the quality of anesthesia care provided.
Anesthesia Management: A Link to Successful Surgeries
In the pursuit of surgical excellence, the role of anesthesia management cannot be overstated. It is a dynamic field where precision, collaboration, and ongoing education converge to ensure the highest standards of patient care. Explore more about the nuances of Anesthesia Management at Anesthesia Management for valuable insights and resources to support optimal surgical outcomes.
In conclusion, optimizing anesthesia management involves a
